The Oral Microbiome & Systemic Disease
Course Number: 561
Course Contents
Introduction
The Human Microbiome Project, which was begun by the US National Institutes of Health in 2007, and completed in 2016, was intended to characterize human microbes and their potential to affect health and disease. These efforts are now helping scientists and clinicians better understand how the human microbiome interacts with the human immune system to either protect or harm the host. One of the major outcomes of this project was the creation of organ-specific data banks, such as the metagenomics of the human intestinal tract, which has the highest number of species, as well as the human oral microbiome database (HOMD), which has the second highest number of microbial species.9 To date, the bank has documented 770+ species while Park et al. have sequenced more than 1,000 species10 and more than 1,200 to 1,500 are suspected.11
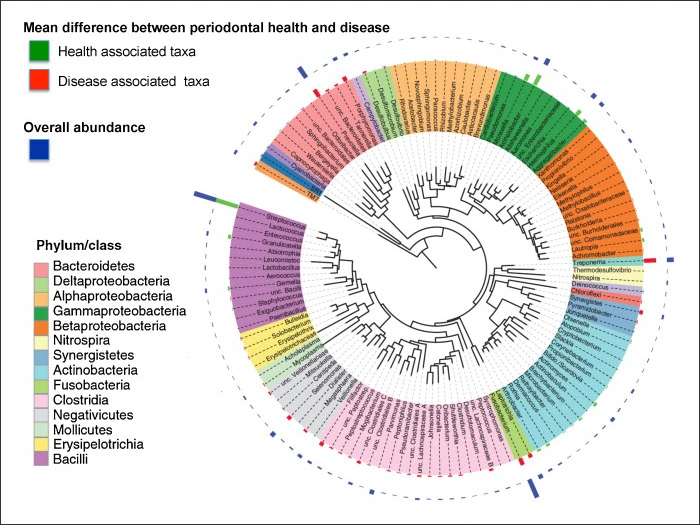
The vast majority of the organisms were not cultured in a lab but were identified through sophisticated genome sequencing technology instead. It is the combination of pathogens, commensals and their associated genomes (genetic material) that make up the oral microbiome. Typically, in a state of health, microbes exist in a symbiotic state, however if this homeostatic balance is disrupted, then a state of dysbiosis occurs. For example, figure 1 provides a visual representation of the microbiome of a periodontal pocket in health and disease.12
Figure 1. Microbiome of Periodontal Pocket in Health and Disease.12
But is it really that simple?
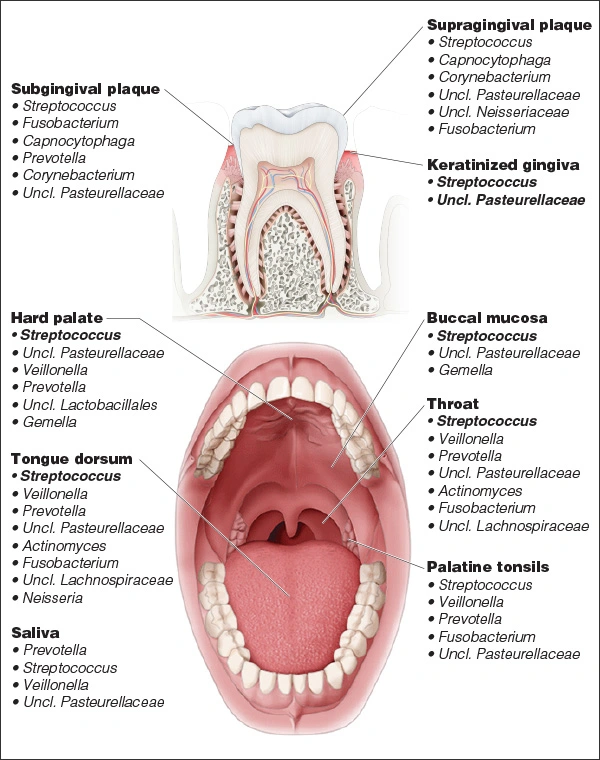
The oral cavity is a multifaceted environment, and this is reflected in the complexity of the microbiome. The composition of the microbiome varies by location in the oral cavity13and that must be taken into consideration when seeking to ascribe some systemic correlation. For example, microbial diversity is different in the floor of the mouth compared to the attached gingiva, and the supragingival microbiome is different from the subgingival microbiome (Figure 2).14 Also, there are a variety of factors, such as the time of day and maturity level of plaque, as well as certain foods, drugs and oral care products that can have a profound effect on the oral microbiome.
Figure 2. Microbial Diversity in the Oral Cavity.15
Why does it matter?
Recently, there has been increased attention on the role of the gut microbiome and how that influences obesity, diabetes and even depression.16,17 There is a huge industry that is centered around the identification of microbes within the gut microbiome and the development of interventional therapies as a result. Yet it is easy to forget that the oral cavity is connected to the gut and is the first exposure of the GI tract. Even more importantly, dental professionals are the experts in the oral cavity and should be aware of more than Streptoccous mutans and Porphyromonas gingivalis and their role on caries and periodontal disease, respectively. In the following sections, we will explore how certain disturbances in the oral microbiome may influence the following systemic diseases:
Diabetes
Heart disease
Hypertension
Stroke
Before doing so, it is important to distinguish between correlation and causation. Correlation refers to a negative or positive association with a systemic illness depending on the presence or absence of certain bacterial species in the microbiome. Basically, correlation is a statistical measure of the linkage between two variables, which can range from a weak to strong correlation. Conversely, if a certain bacterial species causes a particular systemic illness, the etiology of the illness is definitively being attributed to an organism and this requires necessary prospective, randomized data. To date, the current scientific data does not support such a causal association for the systemic health conditions we will evaluate. As systemic illnesses are generally multifactorial in nature, we must always be careful in making statements alluding to causality. Two conditions can be associated without a causative link. These conditions may both have similar risk factors, they may be comorbid with a third condition, or there may be population variables that influence both.