Sleep Apnea Management for the Dentist
Course Number: 578
Course Contents
The Diagnostic Process in OSA
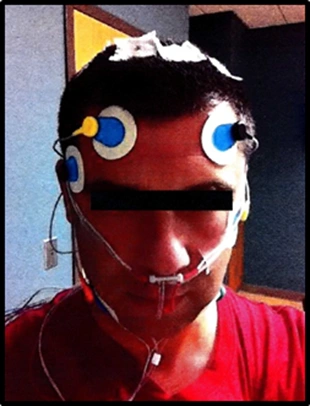
The gold standard in diagnosis of sleep disorders including OSA is an overnight sleep study called a polysomnograph (PSG). PSG components include, but are not limited to, an electroencephalograph (EEG), electromyography (EMG), electrocardiogram (ECG), plethysmography, capnometry and pulse oximetry. The EEG will capture brain activity to determine sleep stage. EMG will capture movement of the eyes and facial muscles such as the chin, to assess REM activity and bruxing events. ECG will check for the presence of arrhythmias. The set up for PSG involves attaching numerous electrodes, sensors and wire leads (as many as 30) to the patient (Figure 3).
Figure 3
A patient preparing for a sleep study at a sleep laboratory.
Freedom of airflow, respiratory effort and oxygen saturation monitoring determine whether the patient is experiencing apneic or hypopneic events. Apnea is the absence of breathing in a period of time while hypopnea is diminished breathing capability within a given time. Apneic and hypopneic episodes both reduce oxygen saturation (hypoxemia), increase carbon dioxide levels (hypercapnia), induce arousals from sleep, and lead to abnormal pauses in breathing. A sleep lab will utilize PSG data to determine the average number of apneas and hypopneas per hour of sleep. This is called the apnea-hypopnea index, or AHI. An AHI of greater than or equal to 5 events per hour would be needed in order to make a diagnosis of OSA.
The severity of OSA is measured by AHI values. The International Classification of Sleep Disorders 3rd Edition (ICSD‑3) in 2014 defined this as the number of obstructive apnea and/or hypopnea events per hour of sleep. 5
| Mild OSA | 5 to 15 events per hour |
| Moderate OSA | > 15 to 30 events per hour |
| Severe OSA | > 30 events per hour |
An AHI of 4.9 or less does not meet the threshold for diagnosis of OSA. The respiratory disturbance index (RDI) is also used in sleep medicine however its definition has varied over the years. RDI uses the same numeric range as AHI to define mild, moderate, and severe OSA; but, in addition to measuring apnea and hypopnea events per hour, RDI also includes less severe respiratory effort-related arousals (RERAs) as part of its scoring.